Prolapse
What is Vaginal Prolapse?
Vaginal prolapse is when structures such as the uterus, rectum, bladder, urethra, small bowel, or the vagina itself may begin to prolapse or fall out of their normal positions. Without medical treatment or surgery, these structures may eventually prolapse farther into the vagina or even through the vaginal opening if their supports weaken enough.
Impact of Prolapse on Anatomy and Health
Prolapse impacts your anatomy by changing the normal positioning of organs. It happens when the muscles and ligaments supporting the organ weaken or stretch. The severity can range from minor, where the organ is only slightly misaligned, to severe, where the organ might protrude externally from the body.
From a health perspective, prolapse can lead to discomfort, pain, urinary or bowel issues, and sexual dysfunction. The condition might also affect mental health due to potential distress and lowered quality of life caused by symptoms.
Causes of Vaginal Prolapse
The primary cause of vaginal prolapse is the strain on the muscles, ligaments, and tissues that support the pelvic organs. This strain can occur due to:
- Vaginal childbirth
- Ageing and lower oestrogen levels after menopause
- Obesity
- Chronic diseases with a heavy cough
- Regular heavy lifting
- Chronic constipation
Symptoms of Vaginal Prolapse
Symptoms can vary depending on the type and severity of the prolapse. They may include:
- A feeling of pressure or fullness in the pelvic area
- A feeling as if you're sitting on a small ball or as if something is falling out of your vagina or anus
- A pulling or stretching sensation in your groyne area or a low backache
- Painful sexual intercourse
- Urinary problems, such as incontinence or incomplete emptying of the bladder
- Constipation or difficulty having bowel movements
- Spotting or bleeding from the vagina
- Increased discomfort when you stand, jump, or lift, and improvement when you lie down
If you suspect that you have a prolapse, it's important to consult a gynaecologist for diagnosis and treatment options.
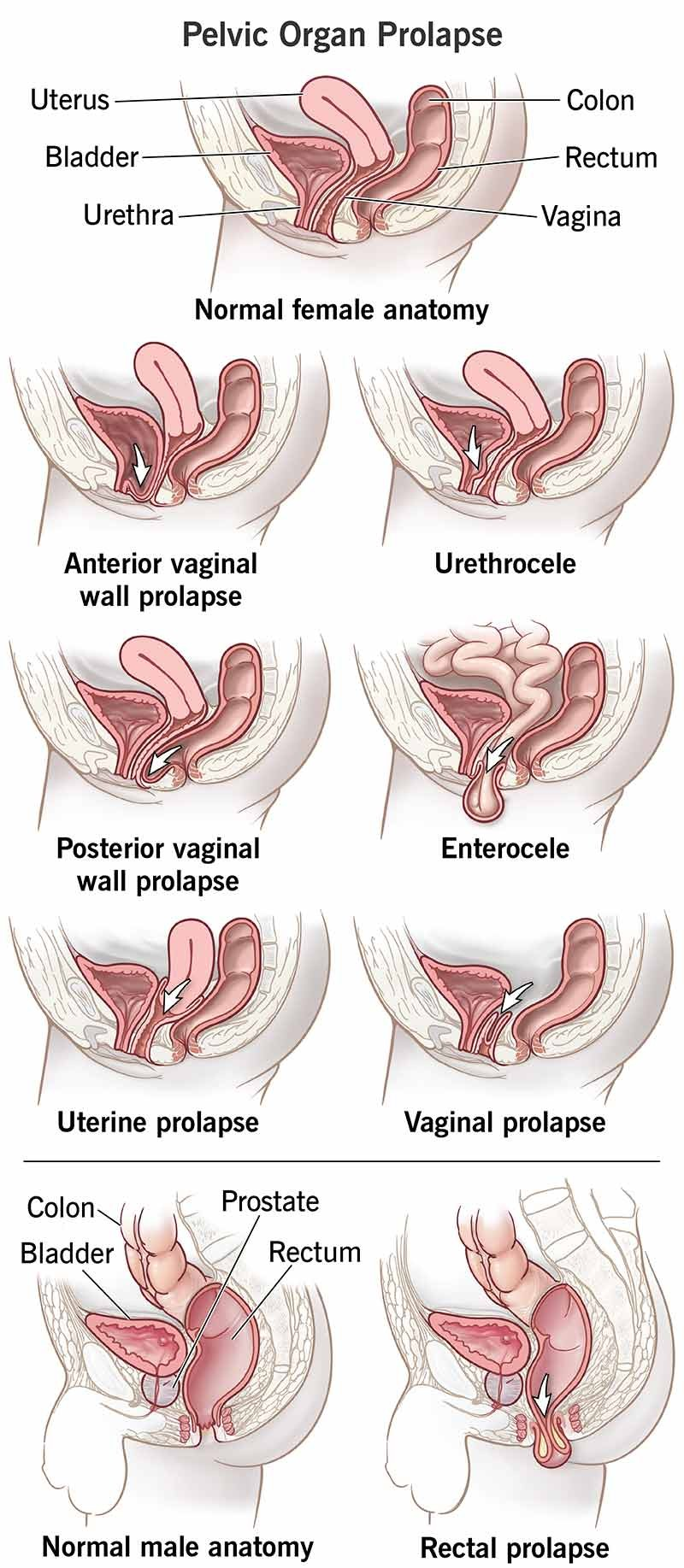
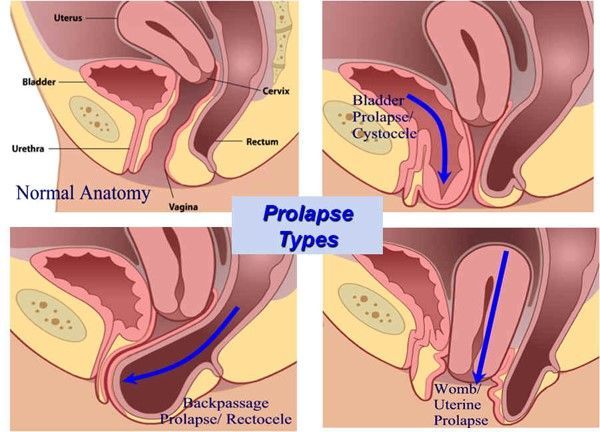
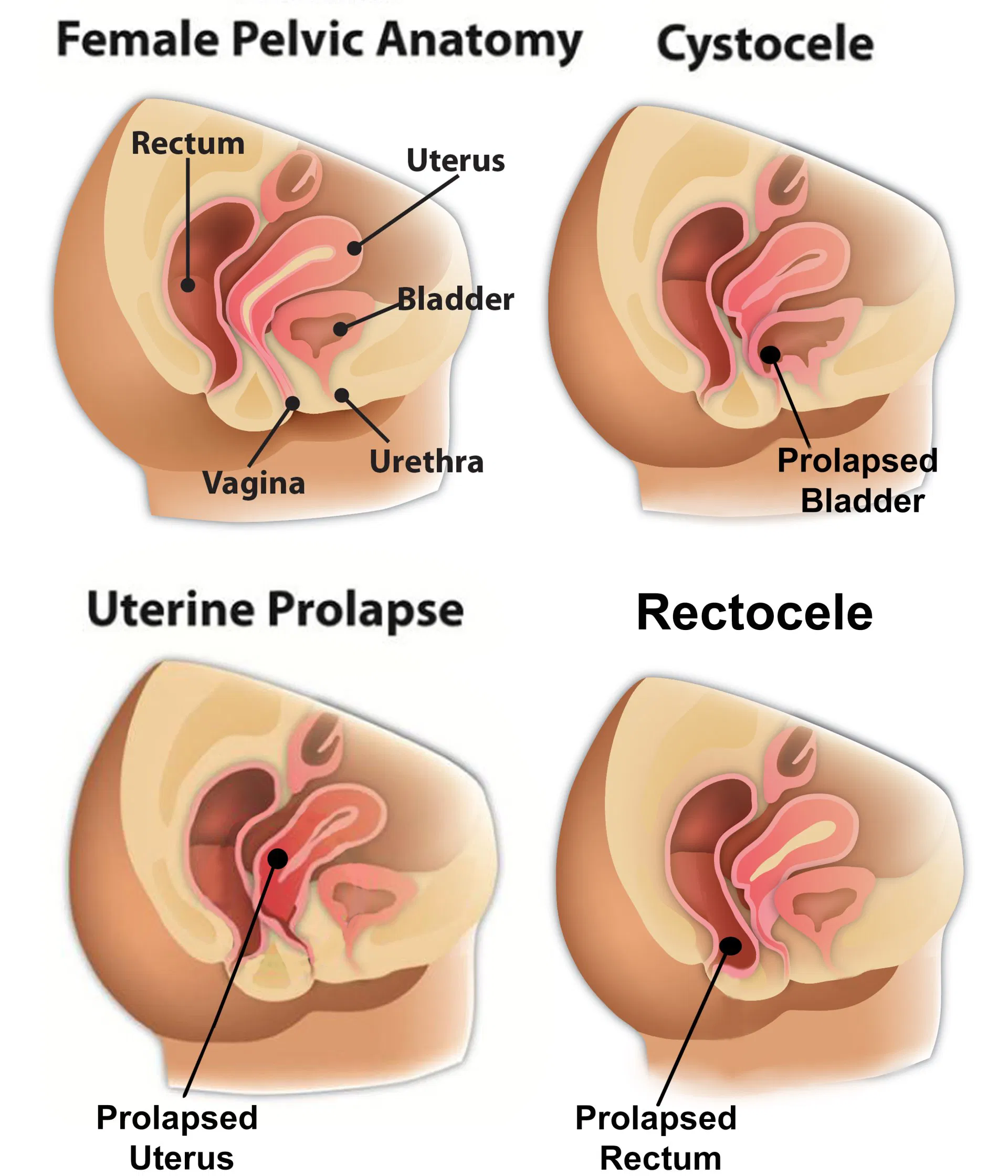
Types of Vaginal Prolapse
- Uterine Prolapse occurs when the uterus sags or slips from its normal position and descends into the vagina. The cause is often the weakening of the muscles and tissues that support the uterus, which can occur due to childbirth, hormonal changes during menopause, or ageing.
- Bladder Prolapse (Cystocele): The bladder descends into the vagina due to the weakening of the tissues between them. The primary symptoms include discomfort and problems with emptying the bladder. This condition is also more common in women who have given birth vaginally.
- Rectal Prolapse: This happens when the rectum, the last part of the large intestine, slips outside the anus. This can result from weakened muscles or ligaments, often due to straining during bowel movements, childbirth, or ageing. It can cause discomfort, difficulty controlling bowel movements, and other problems.
Each of these conditions can vary in severity, with mild cases causing few, if any, symptoms, while more severe cases can cause discomfort, affect daily activities, and require medical intervention. The treatments can include lifestyle changes, pelvic floor exercises, pessary devices, and surgery in more severe cases.
Which Sites Are Affected by Vagina Prolapse?
Vaginal prolapse often affects the anterior (front) and posterior (back) walls of the vagina. Specific types of vaginal prolapse include:
- Cystocele (anterior prolapse): The bladder protrudes into the vagina, causing the front wall to bulge out.
- Rectocele (posterior prolapse): The rectum bulges into the back wall of the vagina.
- Uterine prolapse: The uterus descends into or outside the vagina.
- Vaginal vault prolapse: This happens when the upper portion of the vagina falls toward the vaginal opening, usually following a hysterectomy.
- Enterocele (apical prolapse): Small bowel pushes into the vagina, usually following a hysterectomy.
How Common is Vaginal Prolapse?
Vaginal prolapse is quite common, especially among women with one or more vaginal births. It's estimated that about half of women over 50 have some form of pelvic organ prolapse. However, not all these cases are symptomatic or require treatment.
How Can Vaginal Prolapse Be Avoided?
To reduce the risk of developing a vaginal prolapse, you can:
- Maintain a healthy weight to avoid putting extra pressure on your pelvic floor muscles
- Avoid heavy lifting
- Treat and prevent constipation by eating a high-fibre diet and drinking plenty of fluids.
- Regularly perform exercises to strengthen your pelvic floor muscles (Kegel exercises)
- Avoid smoking, which often leads to chronic coughing
- Get prompt treatment for any conditions that cause intense strain or pressure on the pelvic area, such as bronchitis
What Problems Does Vaginal Prolapse Cause?
Vaginal prolapse can lead to a variety of symptoms, including:
- A feeling of heaviness or dragging in the pelvis
- A bulge in the vagina or a sensation of something coming down your vagina
- Discomfort or pain in the pelvis, lower abdomen, or during intercourse
- Problems with sexual intercourse
- Incontinence or the need to urinate frequently
- Recurrent urinary tract infections
- Constipation or bowel movement difficulties
In severe cases, vaginal prolapse can interfere with daily activities and lead to psychological distress. It's important to seek medical advice if you have symptoms suggestive of vaginal prolapse. Treatment options vary depending on the severity of the prolapse and can range from lifestyle changes and pelvic floor exercises to surgical interventions.
How is Vaginal Prolapse Diagnosed?
A doctor can often diagnose prolapse based on a medical history and a physical examination, including a pelvic exam. The doctor may ask about your symptoms and medical history, including whether you've given birth, had any pelvic surgeries, or have conditions that could increase your risk of prolapse.
During the pelvic exam, the doctor will visually examine your external genitalia, vagina, and possibly rectum to see if any pelvic organs are descending. You may be asked to bear down as if you're trying to push out a baby, which can help the doctor assess how far the organs move when you do this.
Sometimes, additional testing is needed to confirm the diagnosis or check for other problems, such as bladder function tests (urodynamic tests) or imaging tests (ultrasound or MRI).
Non-surgical Treatment of Vaginal Prolapse
- Pelvic Floor Muscle Exercises (Kegels): Strengthening the pelvic floor muscles can help support the pelvic organs. Kegel exercises involve contracting and relaxing the muscles used to control urine flow. Regular and proper execution of these exercises can improve symptoms and prevent further progression of prolapse.
- Lifestyle Modifications: Maintaining a healthy weight, avoiding heavy lifting, and treating constipation can help reduce pelvic floor strain and alleviate prolapse symptoms.
- Pessary Use: A pessary is a device inserted into the vagina to support the prolapsed organs. It helps hold the organs in place and effectively manages prolapse symptoms. Pessaries come in various shapes and sizes and should be fitted and managed by a gynaecologist.
- Physical Therapy: Working with a pelvic floor physical therapist can guide exercises, techniques, and strategies to strengthen the pelvic floor muscles and improve symptoms.
Surgical Treatments for Vaginal Prolapse
Surgical intervention may be considered when non-surgical treatments are ineffective or unsuitable. The specific surgical procedure depends on the type and severity of the prolapse and individual factors. The surgical options can be
- Mesh or Graft Procedures: Synthetic or biological mesh or graft materials may support and reinforce the pelvic floor structures. These procedures may be considered in more complex cases or when traditional repair techniques are unsuitable.
- Mesh Free Surgical Treatments
Mesh Free Surgical Treatment Options
- Vaginal Surgery Repairs using Sutures: Traditional vaginal repair procedures use sutures to restore support to the weakened pelvic floor tissues. The surgeon will make incisions in the vaginal wall and use sutures to tighten and reposition the tissues to their original anatomical position. This procedure aims to repair and reinforce the supportive structures without synthetic mesh.
- Laparoscopic Prolapse Repair: Laparoscopic or minimally invasive surgery can be an option for prolapse repair. This approach involves making small incisions in the abdomen through which specialised surgical instruments and a camera (laparoscope) are inserted. The surgeon uses these instruments to repair and reinforce the pelvic structures, often using sutures or other tissue-supporting techniques. Laparoscopic procedures offer the advantage of reduced scarring, shorter hospital stays, and quicker recovery compared to traditional open surgeries.
- Prolapse Repair with Preserving the Uterus: In cases where the uterus is prolapsed, but the woman desires to preserve it, surgical options are available. These procedures, such as uterine suspension or uterine preservation techniques, aim to correct the prolapse while maintaining the integrity of the uterus. The surgeon will use various techniques, including sutures, to restore support to the uterus and surrounding structures.
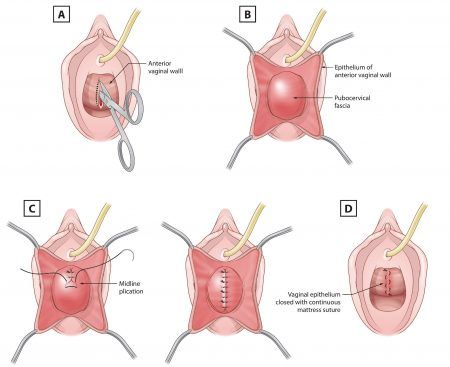
The choice of surgical technique depends on the specific prolapse condition, individual patient factors, and the surgeon's expertise. The decision regarding the most appropriate surgical approach should be made after thorough evaluation and discussion with a gynaecologist or specialist who can provide personalised advice based on the individual situation.
Post Operative Expectations
Most women will require some form of oral analgesia for about one week. Constipation is very common after pelvic floor repair procedures.
Your gynaecologist will give you specific advice on how to address this problem. You should avoid heavy lifting and straining for at least three months.
Your gynaecologist will arrange for you to be reviewed by a physiotherapist with a special interest in pelvic floor disorders. Ongoing pelvic floor exercises and lifestyle modifications to avoid heavy lifting will ensure a long-term cure.
Your gynaecologist may also recommend ongoing use of oestrogen cream to enhance tissue strength and promote healing.
Complications of Vaginal Prolapse Surgery
Every surgical procedure may be associated with certain risks and complications. The possible complications after the surgeries for vaginal prolapse include pain, infection, bleeding, recurrence of symptoms, injury to ureters, and perforation of the rectum and bladder.
The complications are usually mild and can be treated accordingly.
The advantages of choosing minimally invasive surgery are that the defects can be identified, small incisions, reduced postoperative pain and discomfort, shorter hospital duration, and quicker recovery.



