Fibroids
What are Uterine Fibroids?
Uterine fibroids are noncancerous (benign) tumours commonly seen in women of childbearing age. Fibroids are composed of muscle cells and other tissues.
They develop in and around the wall of the uterus or womb wall and can also be found on the exterior wall of the uterus.
Fibroids are composed of muscle cells and other tissues. Uterine fibroids are usually round or semi-round in shape and are found in 30-50% of all women.
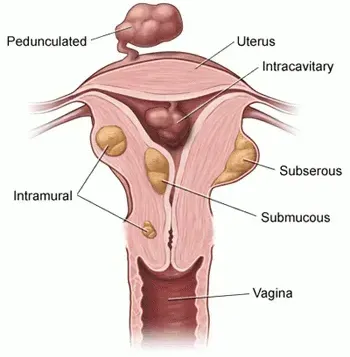
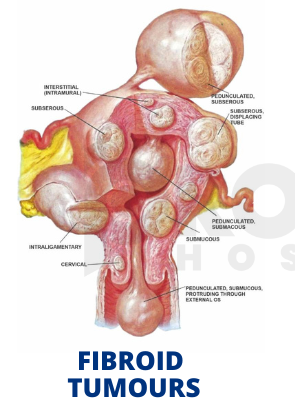
Where Do Fibroids Grow?
Based on their location within the uterus, uterine fibroids can be classified as
- Subserosal fibroids: Sited beneath the serosa (the membrane covering the outer surface of the uterus)
- Submucosal fibroids: Sited inside the uterine cavity below the inside layer of the uterus – the endometrium.
- Intramural fibroids: Sited within the muscular wall of the uterus
- Pedunculated fibroids: Develop on a stalk attached to the outer wall of the uterus
Are Fibroids Common?
Fibroids are a very common type of growth. Approximately 40% to 80% of people with a uterus have fibroids. They occur most often in people between 30 and 50 years old. People who haven’t had their first period (menstruation) yet typically don’t have fibroids. They’re also less common in people who’ve entered menopause.
What Causes Uterine Fibroids?
The exact cause is unknown, but healthcare providers believe the hormones oestrogen and progesterone play a role. Most fibroids happen in people of reproductive age. Studies show that fibroids tend to grow when hormone levels are higher (like during pregnancy) and shrink when hormone levels are low (like during the transition to menopause).
What are the Symptoms of Uterine Fibroids?
The majority of women with uterine fibroids are asymptomatic. Others may experience:
- Prolonged menstrual periods
- Heavy periods
- Pelvic pressure or pain
- Awareness of a pelvic or abdominal mass
- Frequent urination
- Constipation
- Bleeding between periods
- Backache or leg pain
- Difficulty in emptying your bladder
- Difficulty getting pregnant
Some women do not have any symptoms (smaller fibroids).
What are the Risk Factors for Uterine Fibroids?
Several risk factors can play a role in your chances of developing fibroids. These can include:
- Obesity and a higher body mass index (BMI).
- Family history of fibroids.
- Not having children.
- Early onset of menstruation (getting your period at a young age).
- Late age for menopause.
- Fibroids' Impact on Your Health
- In some cases, fibroids can cause complications, including
- Excessive bleeding.
- Excessive menstrual blood loss can cause anaemia. Symptoms of anaemia include breathlessness, fatigue and paleness.
- Pain that becomes unmanageable.
- Swelling of your abdomen or pelvic area.
Large fibroids can press against the bladder, causing a sensation of fullness or discomfort and the need to urinate.
The presence of fibroids can interfere with the implantation of a fertilised egg and cause infertility or difficulty conceiving.
During pregnancy, fibroids can reduce blood flow to the placenta or compete for space with the developing baby. This may result in a miscarriage or premature delivery.
How are Uterine Fibroids Diagnosed?
In many cases, a healthcare provider discovers uterine fibroids during a pelvic exam. Quite often, heavy bleeding and other related symptoms may alert your provider to consider fibroids as a part of the diagnosis. Several tests can be done to confirm fibroids and determine their size and location. These tests can include:
- Ultrasonography: This non-invasive imaging test creates a picture of your internal organs with sound waves.
- Magnetic resonance imaging (MRI): This test creates detailed images of your internal organs using magnets and radio waves.
- Computed tomography (CT) scan: A CT scan uses X-ray images to make a detailed image of your internal organs from several angles.
- Hysteroscopy: During a hysteroscopy, your provider will use a device called a scope (a thin, flexible tube with a camera on the end) to look at fibroids inside your uterus. The scope is passed through your vagina and cervix and then moved into your uterus.
- Hysterosalpingogram(HSG): In this imaging test, your provider places a small catheter in your vagina and then injects saline into your uterus. This extra fluid helps to create a clearer image of your uterus than you would see during a standard ultrasound.
- Laparoscopy: During this test, your provider will make a small cut (incision) in your lower abdomen. A thin and flexible tube with a camera on the end will be inserted to examine your internal organs closely.
Management and Treatments for Fibroids
How are Uterine Fibroids Treated?
Treatment for uterine fibroids can vary depending on the size, number, and location of the fibroids and the symptoms they cause. If you aren’t experiencing any symptoms from your fibroids, you may not need treatment. Small fibroids can often be left alone. Some people never experience any symptoms or have any problems associated with fibroids. In these cases, your provider may recommend monitoring your fibroids with pelvic exams or ultrasounds.
If you’re experiencing symptoms from your fibroids — including anaemia from excess bleeding, moderate to severe pain or urinary tract and bowel problems — you’ll need treatment to help. Your treatment plan will depend on a few factors, including:
- How many fibroids you have.
- The size of your fibroids.
- Where your fibroids are located.
- What symptoms you’re experiencing related to the fibroids.
- Your desire to keep your uterus.
The best treatment option for you will also depend on your future pregnancy plans. Talk to your healthcare provider about your fertility goals when discussing treatment options. Treatment options for uterine fibroids can include:
Medications
- Over-the-counter (OTC) pain medications: These medications help manage pain and discomfort caused by fibroids. OTC medications include acetaminophen and ibuprofen.
- Iron supplements: If you have anaemia from excess bleeding, your provider may also suggest you take an iron supplement.
- Birth control: Birth control can also help with symptoms of fibroids — specifically, heavy bleeding during and between periods and menstrual cramps. There are a variety of birth control options you can use, including oral contraceptive pills, rings, injections and intrauterine devices (IUDs- MIRENA).
- Gonadotropin-releasing hormone (GnRH) agonists: These medications work by shrinking fibroids. They’re sometimes used to shrink a fibroid before surgery, making it easier to remove the fibroid. However, these medications are temporary, and if you stop taking them, the fibroids can grow back.
- Oral therapies: Elagolix is a new oral therapy to manage heavy uterine bleeding in people who haven’t experienced menopause with symptomatic uterine fibroids. It can be taken for up to 24 months. Talk to your provider about the pros and cons of this therapy. Another oral therapy, tranexamic acid, treats heavy menstrual bleeding in people with uterine fibroids.
Talking to your healthcare provider about any medication you take is important. Before starting a new medication, always consult your doctor to discuss any possible complications.
Fibroid Surgery
There are several factors to consider when discussing the different types of surgery for fibroid removal. Not only can the size, location and number of fibroids influence the type of surgery, but your wishes for future pregnancies can also be an important factor when developing a treatment plan. Some surgical options preserve your uterus and allow you to become pregnant in the future, while other options can either damage or remove your uterus.
Myomectomy
Myomectomy is a procedure that allows your provider to remove the fibroids. There are several types of myomectomy. The type of procedure that may work best for you will depend on where your fibroids are located, how big they are and how many you have. The types of myomectomy procedures to remove fibroids can include:
- Hysteroscopy: Your provider inserts a scope (a thin, flexible, tube-like tool) through your vagina and cervix and into your uterus. Your provider uses the scope to cut away and remove the fibroids.
- Laparoscopy: In this procedure, your provider will use a scope to remove the fibroids. Unlike hysteroscopy, this procedure involves placing a few small incisions in your abdomen. This is how the scope will enter and exit your body.
- Laparotomy: During this procedure, your provider makes one larger incision in your abdomen and removes the fibroids through this one cut.
If you aren’t planning future pregnancies, there are additional options your healthcare provider may recommend. These options can be very effective, but they typically prevent future pregnancies. These can include:
Hysterectomy
Your provider removes your uterus during a hysterectomy. A hysterectomy is the only way to cure fibroids. By removing your uterus completely, the fibroids can’t come back, and your symptoms should go away. If your ovaries are left in place, you won’t go into menopause after a hysterectomy. This procedure might be recommended if you’re experiencing very heavy bleeding from your fibroids or if you have large fibroids. Minimally invasive hysterectomies include vaginal, laparoscopic or robotic methods.
Uterine Fibroid Embolization
An interventional radiologist performs this procedure with the help of your gynaecologist. They put a small catheter in your uterine or radial artery and inject small particles, which then block the blood flow from the artery to the fibroids. The loss of blood flow shrinks the fibroids and improves your symptoms. This procedure may not be right for everyone.
Risks to Uterine Fibroid Treatment
There can be risks to any treatment. Medications can have side effects, and some may not fit you well. Talk to your healthcare provider about all medicines you may take for other medical conditions and your complete medical history before starting a new medication. If you experience side effects after starting a new medication, call your provider to discuss your options.
There are also risks involved in the surgical treatment of fibroids. Any surgery places you at risk of infection and bleeding and includes risks associated with anaesthesia. An additional risk of fibroid removal surgery can involve future pregnancies. Some surgical options can prevent future pregnancies. Myomectomy is a procedure that only removes the fibroids, allowing for future pregnancies. However, people who’ve had a myomectomy may need to deliver future babies via C-section. by your surgeon.
Rarely, a myomectomy causes uterine scarring that can lead to infertility.
How large do uterine fibroids need to be before being surgically removed?
There isn’t a definitive size of a fibroid that would automatically mean it needs to be removed. Your healthcare provider will determine if surgery is necessary based on your symptoms. For example, fibroids the size of a small marble may still cause excessive bleeding depending on their location. Your healthcare provider can discuss symptoms that might require surgical intervention.
What happens if fibroids go untreated?
If you don’t have symptoms, treatment for fibroids may not be necessary. If you have large fibroids or your symptoms are causing you pain and discomfort, getting treatment may be the best option. Only you and your provider can decide the best course of treatment or if treatment is necessary.
Prevention
Can Fibroids Be Prevented?
In general, you can’t prevent fibroids. You can reduce risk by maintaining a healthy body weight and getting regular pelvic exams. If you have small fibroids, develop a plan with your healthcare provider to monitor them.
Fibroids and Pregnancy
Because fibroids can grow back, those women planning to become pregnant must try to conceive as early as possible after the myomectomy procedure. However, following surgery, we will advise you to wait at least 6 months until the uterus heals.
Risks During Pregnancy
Studies indicate that the presence of uterine fibroids, depending on their size and location, can increase the risk of complications such as breech presentation, increased chance of Caesarean section, increased bleeding post-delivery of the baby, premature labour and rare growth restriction.
Can I get pregnant if I have uterine fibroids?
Yes, you can get pregnant if you have uterine fibroids. If you already know you have fibroids when you get pregnant, your healthcare provider will work with you to develop a monitoring plan for the fibroids. During pregnancy, your body releases elevated levels of hormones. These hormones support the pregnancy. However, they can also cause your fibroids to get bigger. Large fibroids can cause the following problems during pregnancy:
- Increased risk for a C-section delivery because the foetus can’t flip into a head-down position.
- Labour doesn’t progress.
- Placental abruption.
- Preterm delivery.
Can Fibroids Change Over Time?
Fibroids can shrink or grow over time. They can change size suddenly or steadily over a long period. This can happen for various reasons, but in most cases, this change in fibroid size is linked to the amount of hormones in your body. When you have high levels of hormones in your body, fibroids can get bigger. This can happen at specific times in your life, like during pregnancy. Fibroids can also shrink when your hormone levels drop. This is common after menopause. Often, your symptoms can also get better after menopause.
Will Fibroids Go Away On Their Own?
Fibroids can shrink in some people after menopause. This happens because of a decrease in hormones. When the fibroids shrink, your symptoms may go away. Small fibroids may not need treatment if they aren’t causing any symptoms.
Do fibroids make you tired?
Feeling tired isn’t a common symptom of uterine fibroids. However, it’s a common symptom of anaemia, which can occur when you lose too much blood. Talk to a healthcare provider if you feel excessively tired so they can determine the cause.
Do fibroids make your stomach big?
Yes, it’s possible that large uterine fibroids can cause your stomach to bloat or appear larger.
Living With Fibroids
When Should I Contact My Healthcare Provider?
Contact your healthcare provider if you have symptoms of uterine fibroids, such as:
- Heavy and irregular vaginal bleeding.
- Bleeding between periods.
- Pelvic pain.
- Pain during sex.
- A feeling of pressure or fullness in your belly.
Because these symptoms are common symptoms of other gynaecological conditions, discussing them with a healthcare provider is important.
Are Fibroids Cancer?
It’s extremely rare for a fibroid to go through changes that transform it into a cancerous (malignant) tumour. One out of 350 people with fibroids will develop cancer. No test is 100% predictive in detecting rare fibroid-related cancers. However, people who have rapid growth of uterine fibroids or fibroids that grow after menopause should be evaluated immediately.



