Endometrial Ablation & Hysteroscopy
What is a Hysteroscopy?
Hysteroscopy is a medical procedure in which a thin, lighted tube (called a hysteroscope) is inserted into the uterus through the cervix. The procedure allows a doctor to see the inside of the uterus and diagnose or treat specific conditions. It is commonly used to diagnose and treat issues such as abnormal bleeding, polyps, fibroids, or adhesions, as well as to confirm the placement of an intrauterine device (IUD) or to perform certain types of surgery, such as a biopsy or removal of a growth. It may also be used to assist in the diagnosis of infertility or recurrent miscarriage.
Who is Suitable for Hysteroscopy?
Hysteroscopy is a relatively safe and well-tolerated procedure that can be performed on women of all ages. However, it is most commonly used to diagnose or treat conditions in women of reproductive age.
Hysteroscopy may be recommended for women who are experiencing:
- Abnormal bleeding
- Infertility
- Recurrent miscarriage
- Polyps or fibroids in the uterus
- Adhesions or scar tissue in the uterus
- Uterine anomalies
- Suspected retained products of conception
- Confirmation of the placement of an intrauterine device (IUD)
Benefits of Hysteroscopy
Hysteroscopy is a minimally invasive procedure that can provide several benefits, including:
- Accurate diagnosis,
- Treatment options,
- Minimally invasive,
- Faster recovery time,
- Fewer complications,
- Can help with infertility, and
- Can aid in the diagnosis of recurrent miscarriage
Types of Hysteroscopy
There are two main types of hysteroscopy: diagnostic hysteroscopy and operative hysteroscopy.
- Diagnostic hysteroscopy is used to diagnose polyps, fibroids, and adhesions. The procedure uses a thin, lighted tube called a hysteroscope inserted into the uterus through the cervix. During the procedure, the doctor can see the inside of the uterus and diagnose any issues.
- Operative hysteroscopy treats conditions diagnosed during a diagnostic hysteroscopy. The procedure is performed using the same equipment as diagnostic hysteroscopy, but the doctor will also use specialised instruments to perform surgery, such as removing polyps, fibroids, or adhesions. Operative hysteroscopy can also perform a biopsy, remove a growth, or place an intrauterine device (IUD).
What is Endometrial Ablation?
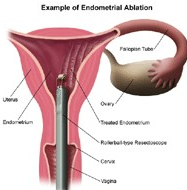
Endometrial ablation is a medical procedure that is used to remove or destroy the endometrial lining of a woman's uterus to reduce or stop menstrual flow. This procedure often treats heavy, prolonged menstrual bleeding that hasn't responded to other treatments.
Who is Suitable for Endometrial Ablation?
Endometrial ablation may be a good option for women who:
- Have prolonged, heavy, or irregular menstrual bleeding.
- Suffer from anaemia due to heavy menstrual flow.
- Have not responded to other treatments such as medication.
- Don't wish to bear children in the future. Pregnancy is possible after endometrial ablation, but it can be dangerous for both the mother and the foetus.
- You can't have or don't want to have a hysterectomy, which is the surgical removal of the uterus.
However, endometrial ablation isn't suitable for everyone. It isn't recommended for women who:
- Have uterine cancer or an increased risk of uterine cancer.
- Have an active genital or urinary tract infection.
- Have an intrauterine device (IUD).
- Have a uterine disorder, such as endometriosis, uterine fibroids, or a recent pregnancy.
Benefits of Endometrial Ablation
The benefits of endometrial ablation include:
- It can significantly reduce menstrual bleeding or stop it entirely.
- It is less invasive than a hysterectomy and avoids the potential side effects and risks of hormones.
- It can often be done as an outpatient procedure without hospitalisation.
- The recovery time is typically short, with most women returning to normal activity within a few days.
Types of Endometrial Ablation
There are several types of endometrial ablation, including:
- Radiofrequency Ablation: This method uses radio waves to create heat which destroys the endometrium.
- Freezing (Cryoablation): This technique uses extreme cold to destroy the endometrium.
- Heated Fluid: In this technique, heated fluid is pumped into the uterus and left in place for about 10 minutes to destroy the endometrial tissue.
- Balloon Therapy involves inserting a balloon into the uterus, which is then filled with heated fluid.
- Microwave: This method uses microwave energy to destroy the endometrium.
What to do Before an Endometrial Ablation?
Before undergoing an endometrial ablation, there are several steps that you should take:
- Understand what the procedure entails, what to expect during recovery, and potential risks and benefits. Make sure all your questions and concerns are addressed.
- Your doctor will review your medical history to ensure you are a suitable candidate for the procedure. This includes your menstrual history, past and current illnesses, medications, and whether you plan to have children.
- A thorough physical and pelvic examination will typically be performed. This may include a Pap smear, ultrasound, or hysteroscopy to examine the uterus and check for abnormalities.
- Certain tests, such as blood tests, may be performed to ensure you are healthy enough for the procedure.
- You may be asked to stop certain medications before the procedure, especially those that can increase the risk of bleeding, like anticoagulants or antiplatelet drugs.
- Some women might be given medications or undergo procedures to thin the endometrium before ablation.
- As you might have some discomfort and bleeding after the procedure, arranging for someone to drive you home and taking it easy for a few days post-procedure is recommended.
- If you're receiving general anaesthesia, you might be instructed to fast — to eat or drink nothing — for several hours before the procedure.
What Happens During an Endometrial Ablation?
During this procedure, a doctor uses a hysteroscope, a thin tube with a light and camera at the end, to look inside the uterus. Here is a typical sequence of events:
- Anaesthesia: Depending on the specifics of the procedure and your overall health, you'll be given either general anaesthesia (you're asleep for the procedure), regional anaesthesia (you're awake, but the lower part of your body is numb), or local anaesthesia (only a small area is numbed).
- Dilation of the cervix: The lower, narrow part of the uterus that connects to the vagina must be dilated or opened to allow the hysteroscope to pass through.
- Insertion of the hysteroscope: The doctor inserts the hysteroscope through the vagina and cervix into the uterus.
- Inspection of the uterus: With the help of the light and camera on the hysteroscope, the doctor inspects the uterus for abnormalities. A saline solution may be pumped through the hysteroscope into the uterus to expand it and provide a clearer view.
- Ablation: After the inspection, an instrument is passed through the hysteroscope to destroy the endometrium (the lining of the uterus). There are several ways to perform this, depending on the specific type of ablation procedure chosen. The methods include heat (thermal ablation), cold (cryoablation), microwave energy, or radiofrequency.
- End of procedure: Once the endometrium has been destroyed, the hysteroscope and other instruments are removed. The procedure usually takes around 30 to 45 minutes.
What to Expect After an Endometrial Ablation?
After the procedure, you may experience side effects such as cramping, slight bleeding, and discharge for several days to weeks. Over-the-counter painkillers can usually manage the pain. It's generally advised to have someone else drive you home after the procedure, and you may need to rest for a few days before returning to your normal activities.
Endometrial Ablation Recovery Plan
As part of your recovery plan, you may be advised to:
- Take over-the-counter pain medications for relief from discomfort or cramps.
- Rest and avoid strenuous activities for a few days.
- Use sanitary pads instead of tampons to manage any discharge or bleeding.
- Avoid sexual intercourse for a period your doctor recommends, usually a few weeks.
- Schedule a follow-up appointment with your doctor to discuss the results and any symptoms or concerns.
Endometrial Ablation Prognosis
Most women have much lighter periods after endometrial ablation, and many stop having periods. The success rate of reducing heavy menstrual bleeding is generally high, and patient satisfaction is typically significant. However, it's crucial to note that endometrial ablation isn't a form of birth control, and pregnancy can still occur, although it can be hazardous and is generally not recommended.
Endometrial Ablation Risks
Endometrial ablation is generally safe but carries some risks, as with any surgical procedure. These can include:
- Pain, bleeding or infection.
- Heat or cold damage to nearby organs.
- A puncture injury of the uterine wall from surgical instruments.
- Rarely, fluid used during the procedure can enter the bloodstream and cause complications.
What if Endometrial Ablation is Delayed?
If endometrial ablation is delayed, the symptoms, such as heavy menstrual bleeding, will likely continue. Due to the ongoing symptoms, this can contribute to anaemia and a lower quality of life. However, delaying the procedure does not typically lead to complications or worsening of the condition. Discussing your symptoms and options with your doctor is crucial.



