Mirena, Copper IUD Insertion
What is an IUD?
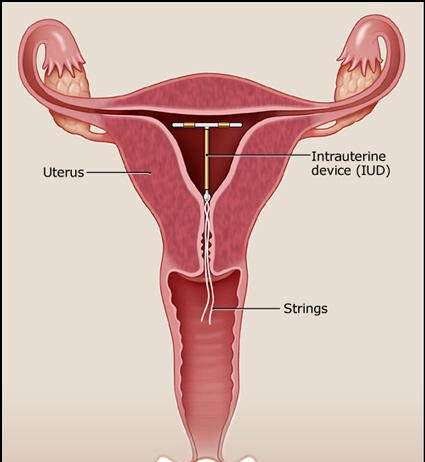
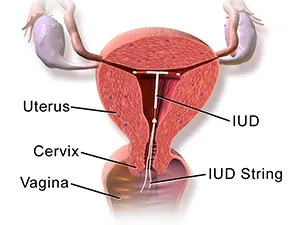
An IUD, or intrauterine device, is a small, T-shaped contraceptive inserted into the uterus to prevent pregnancy. It is one of the most effective and long-lasting forms of reversible contraception available.
Types of IUDs
There are two main types of IUDs available:
- Copper IUD: This type of IUD is made of plastic with a copper wire wrapped around it. The copper acts as a spermicide, creating an inhospitable environment for sperm, thereby preventing fertilisation.
- Hormonal IUD: This type of IUD releases a progestin hormone called levonorgestrel. The hormone thickens the cervical mucus, which inhibits sperm from reaching the uterus, and also thins the uterine lining, making it less receptive to implantation.
What is Mirena?
Mirena is a brand name for a hormonal intrauterine device (IUD) used for contraception. It is a long-acting reversible contraception (LARC) that releases a progestin hormone called levonorgestrel. This hormone is gradually released into the uterus, providing contraception locally.
Mirena is used as:
- a popular type of long-acting, reversible contraception.
- treatment for heavy and painful periods.
Mirena or Copper IUD Insertion Procedure
Both Mirena (a hormonal IUD) and copper IUDs are inserted similarly. The process of inserting the IUD is the same regardless of whether it is a hormonal or copper device. Here are the general steps involved in the insertion of both types of IUDs:
- Preparation: The doctor will start by explaining the procedure and discussing any concerns or questions you may have. They will also review your medical history and perform a pelvic exam if necessary.
- Placement: You will be positioned on an examination table like a pelvic exam. The doctor will insert a speculum into the vagina to visualise the cervix.
- Cleaning and numbing: The cervix and vagina will be cleaned with an antiseptic solution. Sometimes, a local anaesthetic may numb the cervix, although this step is not always necessary.
- Measurement: The doctor will use a special instrument called a sound to measure the depth and position of the uterus. This helps determine the appropriate placement of the IUD.
- Insertion: The IUD is inserted into the uterus through the cervix. It is typically delivered using an insertion tube that protects the IUD during insertion. Once inside the uterus, the IUD is released, and the insertion tube is withdrawn. The arms of the IUD open to form a T shape, securing it in place.
- Trim the strings: After the IUD is in place, the doctor trims the strings attached to the IUD, leaving a small portion extending into the vagina. These strings allow for easy removal of the IUD when desired.
What To Expect After Mirena or Copper IUD Insertion
After the insertion of a Mirena or copper IUD, there are several things you can expect in the following days and weeks. Here are some common experiences:
- Cramping and discomfort: It is normal to experience cramping and discomfort after IUD insertion. This can range from mild to moderate and may last a few hours to a few days. Over-the-counter pain relievers like ibuprofen can help alleviate the discomfort.
- Spotting and irregular bleeding: After IUD insertion, it is common to experience spotting or light bleeding, especially in the first few weeks. This is more pronounced with the copper IUD but can also occur with Mirena. It may take some time for your body to adjust to the IUD, and your bleeding pattern may become irregular initially.
- Changes in menstrual bleeding: Many people experience changes in their menstrual bleeding patterns with Mirena. It may take several months to adjust to the hormonal changes caused by Mirena. With the copper IUD, your menstrual bleeding pattern should remain relatively unaltered.
- Monitoring the strings: After IUD insertion, it's important to check the strings regularly to ensure that the IUD is in place. You can do this by inserting a clean finger into your vagina and feeling for the strings, which should be at the cervix. If you can't feel the strings or if they feel significantly longer or shorter than usual, contact your doctor.
- Follow-up appointments: Your doctor may schedule a follow-up appointment to ensure that the IUD is properly positioned and to address any concerns or questions you may have. They may also check the strings during this visit.
If you have any severe or persistent pain, heavy bleeding, fever, or other concerning symptoms after IUD insertion, it is important to contact your doctor for evaluation.
Potential Risks of IUD Insertion
While intrauterine devices (IUDs) are generally safe and well-tolerated, they carry potential risks and complications. Knowing these risks is important before choosing an IUD as a contraceptive method. Here are some potential risks associated with IUD use:
- Expulsion: IUD expulsion occurs when the device comes out of the uterus. This can happen shortly after insertion or at any time while the IUD is in place. Expulsion rates vary depending on factors such as the type of IUD and individual characteristics. If you suspect expulsion, contact your healthcare provider.
- Perforation: In rare cases, IUD insertion can lead to uterine perforation, where the IUD punctures the uterine wall. This can cause severe pain or discomfort. The risk of perforation is higher during insertion and is influenced by factors such as the skill of the healthcare provider and the position of the uterus. If you suspect perforation, seek immediate medical attention.
- Infections can occur during or after IUD insertion, although the risk is relatively low. The insertion process can introduce bacteria into the uterus, potentially leading to pelvic inflammatory disease (PID) or other uterine infections. Signs of infection may include severe pain, fever, chills, or abnormal vaginal discharge. If you experience any of these symptoms, seek medical attention promptly.
- Expelled or embedded strings: The strings attached to the IUD may be expelled from the cervix or embedded in the cervical canal. This can make removal or checking the position of the IUD more challenging. If you notice any changes in the location or accessibility of the strings, consult your healthcare provider.
The overall risks of IUD use are relatively low, and many individuals tolerate IUDs well without experiencing complications. Before deciding on an IUD, consult a gynaecologist to discuss your medical history, individual risk factors, and concerns.
Effectiveness of IUDs
Both Mirena (a hormonal IUD) and copper IUDs are highly effective methods of contraception. However, they have different mechanisms of action and vary slightly in their effectiveness. Here's a comparison of their effectiveness:
Mirena (Hormonal IUD)
- Typical failure rate: Less than one pregnancy per 100 women in a year of use.
- Perfect use failure rate: Less than one pregnancy per 1,000 women in a year of use.
- Mirena is one of the most effective forms of contraception available.
Copper IUD
- Typical failure rate: Less than one pregnancy per 100 women in a year of use.
- Perfect use failure rate: Less than one pregnancy per 100 women in a year of use.
- Copper IUDs are also highly effective at preventing pregnancy.
The effectiveness of both IUD types largely depends on correct and consistent use. Perfect use refers to following the instructions precisely, while typical use accounts for human error or inconsistencies.
How Long Do IUDs Last?
Mirena is typically effective for up to 5 years, while copper IUDs can be effective for up to 10 years, depending on the specific brand.



