Bladder Treatments
What are Bladder Problems?
Bladder problems typically refer to conditions that interfere with the normal functioning of the bladder, causing symptoms such as pain, discomfort, and changes in urinary habits. These conditions can be due to issues with the bladder's muscles, nerves, or tissues, infections, or other underlying health problems.
Common Bladder Problems
The most common bladder problems include:
- Urinary stress incontinence
- Overactive bladder
- Recurrent urinary tract infections
- Bladder pain syndrome and interstitial cystitis
Urinary Stress Incontinence
What is Urinary Stress Incontinence?
Urinary stress incontinence is a common condition where urine involuntarily leaks out when the bladder is under pressure – for example, when coughing, sneezing, or exercising. It's often caused by weakness of the muscles that control urination.
Treatments for Urinary Stress Incontinence
There are a few surgical treatments for Urinary Stress Incontinence, including:
- Urethral Sling Procedures: These are commonly performed to treat stress urinary incontinence. In these procedures, a sling is made of synthetic material or the person's tissue and is placed around the urethra and the neck of the bladder to provide support. This helps keep the urethra closed, especially when there's increased abdominal pressure (like when you cough or sneeze), so urine doesn't leak out.
- Burch colposuspension: This surgical procedure treats stress incontinence by supporting the urethra. In this procedure, sutures are attached to the vaginal wall and ligaments close to the pubic bone, creating a supportive hammock for the bladder, neck and urethra.
- Urethral Bulking Agents: These substances are injected into tissues around the urethra. The bulking agent helps to "plump up" the urethral tissue and helps the sphincter of the urethra close more effectively, thereby reducing urine leakage.
Sling procedures and Burch colposuspension tend to have good long-term success rates, but they also carry the risks associated with surgery, such as infection or injury to nearby organs. Bulking agents are less invasive but may not last as long and must be repeated.
Overactive Bladder
What is an Overactive Bladder?
Overactive bladder (OAB) is a condition characterised by a sudden urge to urinate, which can be difficult to control. Symptoms may include urgency, frequency (needing to urinate more often than usual), nocturia (waking up multiple times during the night to urinate), and in some cases, urge incontinence (involuntary leakage of urine).
Treatments for Overactive Bladder
Treatment options for overactive bladder are designed to manage these symptoms and improve quality of life. Here are some common treatments:
- Behavioural Techniques include bladder training, pelvic floor exercises, and lifestyle modifications. Bladder training involves timed voiding to extend the time between urination gradually. Pelvic floor exercises (Kegel exercises) can strengthen the muscles that control urination. Lifestyle modifications can include changes in diet (avoiding bladder irritants), fluid management, and regular exercise.
- Medication: Several medications treat overactive bladder, including anticholinergics and beta-3 adrenergic agonists. These medications help to relax the bladder muscle, reducing symptoms of urgency and frequency.
- Botox Injections: Botox can be injected into the bladder muscle, causing it to relax and increase its storage capacity while reducing urinary incontinence episodes.
- Nerve Stimulation: Sacral nerve stimulation involves using a small device implanted under the skin to send electrical impulses to the sacral nerves, which play a role in bladder function. Percutaneous tibial nerve stimulation (PTNS) is a less invasive form of nerve stimulation that sends impulses through a nerve in the ankle up to the sacral nerves.
- Surgery: In severe cases, surgical interventions may be considered. These are typically reserved for cases where other treatments have failed and can include augmentation cystoplasty (expanding the bladder using a piece of the intestine) or urinary diversion (creating a new route for urine to exit the body).
Recurrent Urinary Tract Infections
What is Recurrent Urinary Tract Infection?
Recurrent urinary tract infections (UTIs) are defined as having at least two infections in six months or three in a year. UTIs occur when bacteria enter the urinary tract, typically through the urethra, and begin to multiply in the bladder.
Although the urinary system is designed to keep such invaders out, they sometimes fail. UTIs are often caused by Escherichia coli (E.coli), a bacteria found in the gastrointestinal (GI) tract.
Common symptoms include a strong, persistent urge to urinate, a burning sensation during urination, passing frequent but small amounts of urine, urine that appears cloudy, urine that appears red or bright pink (a sign of blood in the urine), strong-smelling urine, and pelvic pain (in women).
Treatments for Recurrent UTIs
Treatment of UTIs typically involves antibiotics to kill the bacteria causing the infection. If you're experiencing recurrent UTIs, your doctor may recommend the following:
- Low-dose antibiotics, initially for six months but sometimes longer, to prevent new infections.
- Single-dose antibiotics after sexual intercourse if your infections are related to sexual activity.
- Antibiotics for 1 or 2 days every time symptoms appear.
- A non-antibiotic prophylaxis therapy, such as topical oestrogen therapy for postmenopausal women.
- Self-diagnosis and treatment, if you stay in touch with your doctor. You may be asked to take a single dose of an antibiotic after symptoms appear, even before a lab test confirms a UTI.
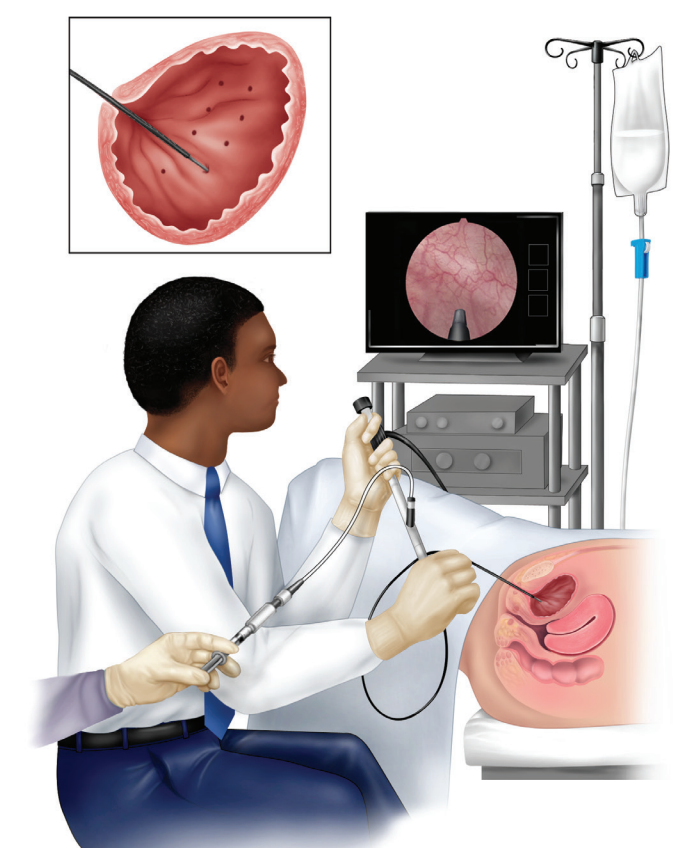
- Intravesical instillation of medication involves placing a medication directly into the bladder through a catheter to prevent infections. This is usually done in more severe or complicated cases.
Recurrent UTIs can also be managed through lifestyle changes like drinking plenty of water, urinating regularly and after sexual intercourse, and - for women - wiping from front to back to prevent bacteria in the anal region from spreading to the vagina and urethra.
Bladder Pain Syndrome
What is Bladder Pain Syndrome?
Bladder pain syndrome, or interstitial cystitis, is a chronic bladder condition. It's characterised by pain and pressure in the bladder and lower urinary tract symptoms that last for six weeks or more without an infection or other clear cause.
Symptoms may include:
- Chronic pelvic pain.
- A persistent, urgent need to urinate.
- Frequent urination, often of small amounts, throughout the day and night.
- Pain or discomfort while the bladder fills and relief after urinating.
- Pain during sexual intercourse.
The cause of interstitial cystitis isn't well understood, but it's thought to involve a defect in the bladder's protective lining (epithelium). Multiple factors likely contribute to the condition.
Interstitial cystitis can be difficult to diagnose because its symptoms often mimic other conditions, including urinary tract infections, bladder cancer, endometriosis in women, and prostatitis in men.
Treatments for Bladder Pain Syndrome
Treatments for bladder pain syndrome or interstitial cystitis include:
- Physical therapy: Pelvic floor physical therapy might be recommended to help alleviate certain types of pelvic pain.
- Oral medications: Nonsteroidal anti-inflammatory drugs can help relieve pain. Antihistamines or pentosan polysulfate sodium may help reduce urinary urgency and frequency and relieve pain.
- Nerve stimulation: Electrical nerve stimulation can help alleviate symptoms, particularly those of urgency, frequency, and pain.
- Bladder distention: This is sometimes done as part of diagnosing the condition. Some people find this procedure provides temporary relief from symptoms.
- Intravesical medication: Medication is placed directly into the bladder to help relieve symptoms.
- Surgery: This is reserved for people with severe pain who haven't responded to other treatments and often involves diverting urine flow or enlarging the bladder.
Lifestyle changes such as stress management, diet modifications (avoiding foods that seem to worsen symptoms), smoking cessation, and gentle exercise can also help manage the symptoms of this condition.
Who is Suitable for Bladder Treatments?
An otherwise healthy person with a mild overactive bladder might start with lifestyle changes and bladder training, while someone with severe urinary incontinence might require surgery. In the case of bladder cancer, treatment will depend on the stage and grade of the cancer, as well as the patient's overall health and personal preferences.
Always consult a doctor to understand the best treatment options for any bladder condition.
Benefits of Bladder Treatments
Bladder treatments can significantly improve a person's quality of life by relieving uncomfortable and sometimes distressing symptoms.
Benefits of bladder treatments may include:
- Improvement in symptoms
- Better sleep
- Improved quality of life
- Prevention of complications
Bladder Treatments Prognosis
Here are some common prognoses associated with bladder treatments:
- Medications: Many people with conditions like overactive bladder or urinary incontinence see significant improvement in their symptoms with medication. However, medications may not work for everyone, and some may experience side effects.
- Behavioural modifications and physical therapy: These treatments often have very good outcomes, especially when performed consistently and correctly. They can be particularly effective for stress urinary incontinence and overactive bladder.
- Surgery: Surgical procedures generally have success rates. For example, sling operations for stress incontinence are often very effective. For bladder cancer, the prognosis can vary significantly depending on the stage and grade of the cancer.
Bladder Treatments Risks
The risks of bladder treatments also depend on the type of treatment. Here are some common risks:
- Medications that treat overactive bladder can sometimes cause dry mouth, constipation, and blurred vision.
- All surgeries carry some risk, including infection, bleeding, and damage to nearby organs. There's also the risk of anaesthesia and the potential for complications related to other health conditions. Some surgeries, such as those for bladder cancer, may require significant recovery and lifestyle changes.
- Physical therapy and behavioural modifications generally carry very low risk. However, pelvic floor exercises must be performed correctly to be effective and to avoid worsening symptoms.
What if Bladder Treatments are Delayed?
Depending on the specific condition, delaying treatment for bladder conditions can lead to various consequences. Below are several potential consequences:
- Increased discomfort and disruption
- Possible kidney damage
- Progression of bladder cancer
- Increased risk of complications
- Psychosocial effects
- Economic implications
Therefore, seeking medical attention is important if you're experiencing bladder issues. Prompt diagnosis and treatment can alleviate symptoms, improve quality of life, and prevent complications.



