Endometriosis & Adenomyosis
What is Endometriosis?
Endometriosis is a common gynaecological condition in women of reproductive age. The average age of diagnosis is 27 years.
It occurs when the glandular tissue of the inner lining of the uterus (endometrium) grows outside the uterus.
Unfortunately, women spent several years searching for the cause of their pain and infertility before receiving the diagnosis of endometriosis.
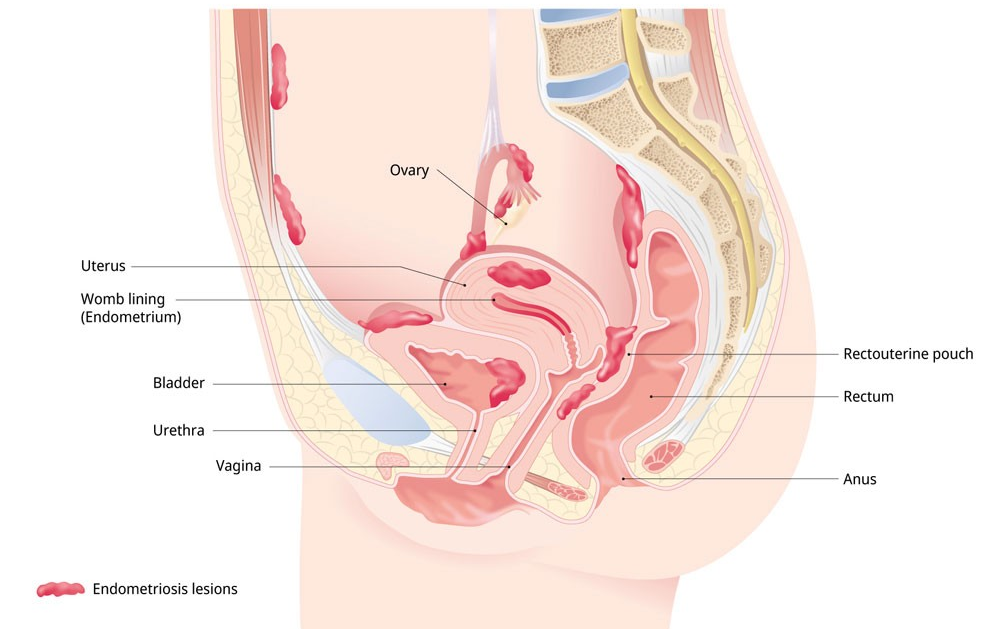
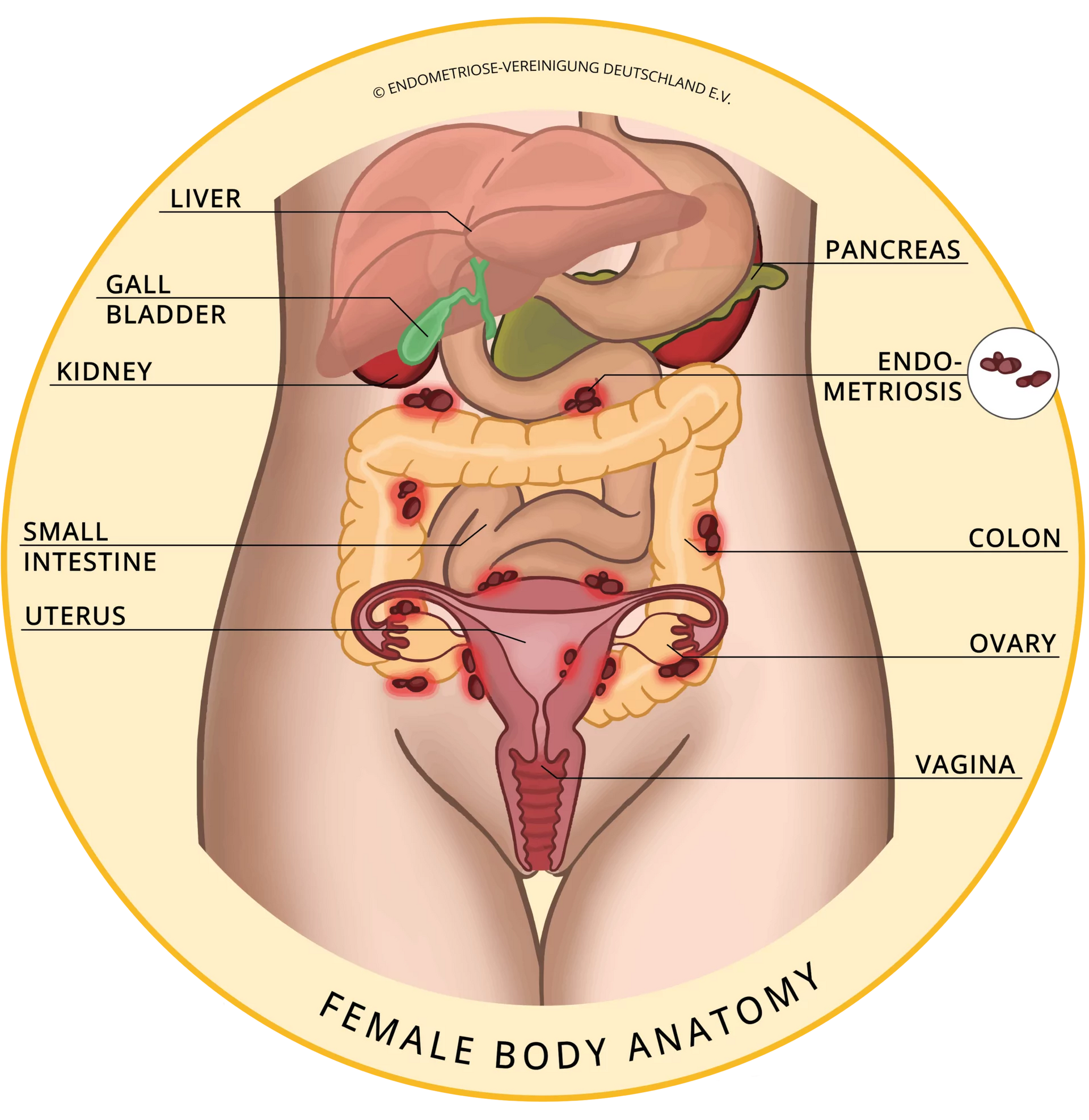
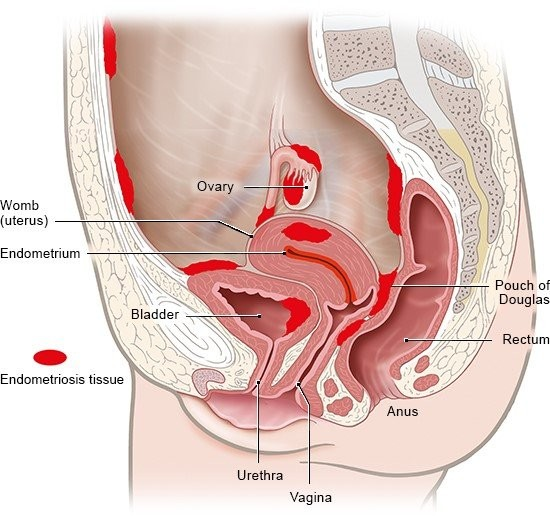
Where does Endometriosis Occur?
Endometriosis can occur in the pelvic organs, which include
- ovaries,
- the outer surface of the uterus,
- the Fallopian Tubes,
- the lining of the pelvic cavity,
- the tissues that hold the uterus in place (uterosacral ligaments).
It can also involve the vagina, cervix, vulva, bladder and bowel (including the rectum and appendix).
In rare cases, it has been found in other body parts, such as the diaphragm, lungs, brain and skin.
How Does Endometriosis Affect Women?
Endometriosis is:
- one of the top three causes of female infertility
- the most common cause of pelvic pain in women between ages 10 and 50 years.
Causes of Endometriosis
The exact cause of endometriosis is not known. Popular theories include
- Retrograde menstruation (the blood flows into the pelvic cavity instead of outside through the vagina),
- Genes have been isolated, which are associated with severe endometriosis. Endometriosis can be associated with a defect in the immune system, and
- Other factors, including stress, dioxins and xenoestrogens, could aggravate symptoms. They are not valid concepts of aetiology.
No theory explains all the findings.
Symptoms of Endometriosis
Patients may experience various levels of
- pain in the lower abdomen, back or in pelvis during menstruation,
- pain during intercourse,
- heavy menstrual bleeding,
- abnormal bleeding between periods,
- painful bowel movements or urination,
- infertility. and
- tiredness/fatigue.
Diagnosis of Endometriosis
Endometriosis may be suspected in medical history. Your doctor will
- ask you about your general health and symptoms,
- perform a pelvic examination to feel for the presence of large cysts or scars, and
- an ultrasound scan may also be performed to look for ovarian cysts (endometriomas).
A definitive diagnosis can only be made by laparoscopy to gain visual confirmation, so it is often delayed several years from the onset of symptoms.
- If endometriosis is suspected, an ultrasound will be requested to assess for severe endometriosis. Occasionally, MRI or CT scans will also be requested. Only a few ultrasound providers specialise in endometriosis, and we may refer you to one of these.
- Laparoscopy is the only way to confirm the diagnosis of endometriosis by visualising it during laparoscopy. A diagnostic laparoscopy (key-hole surgery) is a day procedure under general anaesthesia. Laparoscopy involves a long, thin camera inserted through an incision in the abdomen. A biopsy is often taken for histopathological testing.
Treatment for Endometriosis
Pain Medication for Endometriosis
Over-the-counter pain relievers, such as non-steroidal anti-inflammatory medications or Paracetamol, may be helpful for mild pain.
Other forms of analgesia may be required.
Hormonal Treatment for Endometriosis
Hormone treatment is recommended for mild endometriosis symptoms. This can be the oral contraceptive pill, mini pill, Implanon, Progesterone-based IUD or injections. Visanne is a progestogen pill used to treat endometriosis but is not considered a contraceptive.
Hormone treatment can suppress the activity of endometriosis or decrease recurrence after surgical treatment. This is not appropriate when trying to conceive.
Surgery for Endometriosis
Surgery is the best option for women with infertility and those with severe pain.
Surgery is an option for women who have:
- large cysts
- severe pain
- fertility problems
- pain during intercourse
Laparoscopic Treatment of Endometriosis
Endometriosis surgery is most often done laparoscopically. Endometriosis can be treated with diathermy (burning) or removed if endometriosis is present. Excision of endometriosis is known to be the optimal treatment for endometriosis.
- Laparoscopy has also been shown to improve fertility. An increased pregnancy rate is observed for up to 12 months following the excision of endometriosis. Some women may still require IVF to achieve pregnancy.
- Laparoscopic Uterosacral Ligament Excision
Hysterectomy
Pelvic clearance operation and hysterectomy is another option reserved for women who do not desire fertility or experience severe symptoms.
Hysterectomy involves the removal of the uterus. It is done when there is significant pain and generally when other options have failed.
What is Adenomyosis?
Adenomyosis is a rare disease where the inner lining of the uterus (endometrium) breaks through the uterus muscle wall (myometrium).
The endometrium cells invade and destroy the uterine tissue, causing scarring and infertility.
It is also known as adenomyomatosis, adenomyosis uteri, internal endometriosis, adenomatous endometriosis, and uterine endometriosis.
Adenomyosis is sometimes confused with endometriosis, where endometrial tissue grows outside of the uterus and with fibroids and leiomyomas, which are benign uterus tumours. However, these conditions are distinct from adenomyosis and should be evaluated separately.
Adenomyosis differs from endometriosis when the same tissue grows in other parts of the body outside the uterus.
It can cause pain in your abdomen or pelvis, irregular periods, and heavy bleeding. It can also affect fertility because it can interfere with the implantation of a fertilised egg into the uterine wall.
How Does Adenomyosis Impact Your Anatomy and Health?
Adenomyosis can impact your anatomy and health in many ways.
It can cause an enlarged uterus, which can cause pressure on other organs in the pelvic area,
- severe pain and cramping, especially during menstruation
- heavy menstrual bleeding,
- heavy and prolonged menstrual bleeding,
- pain during intercourse, and
- infertility if left untreated.
Adenomyosis symptoms can be managed effectively with the right diagnosis and treatment plan with hormonal therapy, pain medications, and surgery.
Who is Most at Risk for Adenomyosis?
Adenomyosis affects about 2% of women, usually between 30 and 50.
More specifically, women are at increased risk for Adenomyosis if they are
- Aged 40 to 50,
- Delivered children, especially twins or caesarean sections because, during childbirth, muscles within the uterus can be damaged,
- Undergone in-vitro fertilisation, where you take eggs from the woman and fertilise them in a petri dish, and
- Have a family history of adenomyosis.
Additionally, women with endometriosis and heavy periods are at greater risk of developing the condition.
Although there is no definitive way to prevent adenomyosis, knowing and being mindful of the risk factors can help reduce the likelihood of developing this condition.
What are the Types of Adenomyosis?
There are two types of adenomyosis:
- Diffuse adenomyosis - Diffuse adenomyosis occurs when the endometrial tissue is distributed throughout the uterine wall
- Focal adenomyosis - when the endometrial tissue is localised in one area of the uterus.
Both types of adenomyosis can cause similar symptoms, but they may require different treatments.
What are the Symptoms of Adenomyosis?
Symptoms of Adenomyosis are
- heavy menstrual periods,
- infertility, and
- pain during intercourse.
The primary symptom of adenomyosis is abnormal uterine bleeding, which may include heavy, prolonged, and painful periods. Other symptoms may include abdominal cramping and discomfort, painful intercourse, and spotting between periods.
Additionally, some women may experience fatigue, back pain, and digestive issues if adenomyosis is left untreated. It is important to be aware of these symptoms and seek medical help if they occur.
The most common symptoms of adenomyosis are heavy menstrual bleeding, pelvic pain, and cramping. Other symptoms may include fatigue, back pain, and bloating.
What are the Causes of Adenomyosis?
The exact cause of adenomyosis is unknown, but it is believed to be linked to:
- Hormonal imbalances (oestrogen),
- Endometrial cell disruption
- Pelvic inflammatory disease,
- Genetic factors, and
- Environmental factors and certain cancer treatments.
It usually goes away after menopause when your oestrogen levels drop.
Adenomyosis may also result from uterine trauma, such as caesarean section and endometrial tissue growing into the uterine wall.
What is the difference between adenomyosis and endometriosis?
Adenomyosis and endometriosis are disorders involving endometrial-like tissue. Both conditions can be painful, but adenomyosis is more likely to cause heavy menstrual bleeding. The difference between these conditions is where the tissue grows.
- Adenomyosis: Endometrial-like tissue grows into the muscle of your uterus.
- Endometriosis: Endometrial-like tissue grows outside your uterus in places like your ovaries or fallopian tubes.
Is Adenomyosis a Serious Condition?
Adenomyosis doesn’t usually cause any serious complications. It can lead to difficulty conceiving or miscarriage. The symptoms it causes can disrupt your daily life. Don’t be afraid to talk to your healthcare provider about ways to feel better.
What are the Dangers of Adenomyosis?
There aren’t any life-threatening dangers of adenomyosis. It can cause heavy bleeding, prolonged menstrual bleeding and pelvic pain.
What are the Stages of Adenomyosis?
Adenomyosis is typically divided into four stages, depending on the severity of the condition.
- Asymptomatic: In this stage, the patient does not experience symptoms but may have a larger-than-normal uterus on an ultrasound.
- Symptomatic: In this stage, the patient will experience pain in the lower abdomen, heavy periods, and during intercourse.
- Severe Symptoms: In this stage, the patient will experience more severe symptoms such as infertility or bladder problems.
How is Adenomyosis Diagnosed?
Adenomyosis is a type of endometriosis that can be hard to diagnose.
Often diagnosing Adenomyosis occurs after ruling out other symptomatic causes, such as leiomyomas, endometriosis, and uterine polyps.
Adenomyosis is usually diagnosed by
- Taking a patient’s history.
- Performing a pelvic exam that reveals an enlarged, tender uterus
- Ultrasound imaging of the uterus
- Magnetic resonance imaging (MRI) of the uterus
- Biopsy after a hysterectomy
During a pelvic examination, the doctor will inspect the uterus for abnormal changes or growth. An ultrasound may further examine the uterus and confirm the diagnosis.
Can adenomyosis become cancerous?
No. Adenomyosis itself doesn’t cause cancer or lead to cancer
How Can Adenomyosis Be Treated?
The treatment of Adenomyosis can vary from person to person. The type of treatment will depend on the severity of the adenomyosis and may include:
- Anti-inflammatory medications,
- Hormone therapy, or
- Surgery.
Surgery may be recommended in some cases to remove the endometrial tissue from the uterus.
In addition, some women may find relief from natural treatments, such as dietary changes, exercise, and complementary therapies, such as acupuncture.
Medical Therapy for Adenomyosis
- Hormonal therapy can involve combining oestrogen-progestin birth control pills, hormone-containing patches, or vaginal rings to help regulate blood flow during periods and reduce pain.
- Non-hormonal therapy to control inflammation and reduce pain using pelvic rest and NSAIDs such as ibuprofen or naproxen.
Surgical Treatment for Adenomyosis
If your pain is severe and no other treatments have worked, surgery to:
- Remove abnormal areas of the muscle layer of your uterus
- Remove the lining of the uterus (Endometrial Ablation) or
- Remove the uterus (Hysterectomy) for severe adenomyosis who have not responded to other treatments.
What if Adenomyosis is Untreated?
Women need to know what Adenomyosis is and the risks associated with it. This way, they can be proactive in getting treatment or at least ensure they know how to identify the symptoms and when to get help.
If untreated, the condition can cause severe and prolonged pain. It can also cause complications such as
- infertility
- increased risk of miscarriage.
This is because the embryo can’t implant into your uterine lining.
Other problems may include chronic pelvic and abdominal pain.
Living With
When should I call a healthcare provider?
You should call your healthcare provider if you experience:
- Extremely heavy periods
- Severely painful cramps
- Painful intercourse
- A feeling of fullness or heaviness in your abdomen
Outlook / Prognosis
What can I expect if I have this condition?
Many people who experience life-disrupting symptoms from adenomyosis find relief through treatment. After menopause, symptoms should go away. But you may still have an enlarged uterus.
How does adenomyosis affect pregnancy?
Adenomyosis tends to affect women who have had at least one child. However, the condition may make it difficult to conceive for the first time or to have another child. Once you’re pregnant, there’s an increased risk of:
- Miscarriage
- Premature labour
Why Consider Taking Action for Adenomyosis?
Taking action for adenomyosis is important to reduce the severity of symptoms and prevent any possible complications.
The earlier the diagnosis and treatment, the more effective it will be.
Treatment options such as medications, surgery, and natural therapies can help manage symptoms and improve the quality of life for those affected by adenomyosis. Therefore, it is essential to know the symptoms, risk factors, stages, and treatments for adenomyosis to ensure proper care is taken if it is ever diagnosed.
Adenomyosis can be a debilitating condition, and it is important to take action if you are experiencing any of the symptoms. Treatment can help reduce pain and improve quality of life.



